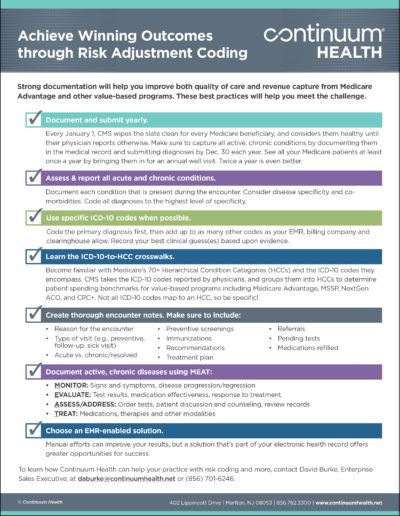
Physicians must code diagnoses properly to succeed under Medicare & other value-based contracts
Each year, CMS sets cost benchmarks for every Medicare member, based on the patients’ diagnoses during the prior year. But what if the physician hasn’t reported their patients’ health information accurately or fully? The result is often benchmarks that are set too low, and costs of care exceeding benchmarks.
The payer then thinks the provider spent too much on members’ care, and does not recognize or reward the value (high quality/lower cost) of the care provided by the physician.
That’s why proper Medicare risk adjustment coding—entering diagnosis codes in the EMR and on claims—is essential. Providers who follow best practices for risk adjustmentcoding have a better chance of earning shared savings.
“Accurate and appropriate documentation with specific coding indirectly affects patient care through reimbursement. This in turn affects the amount of resources available to the patient.” – Dr. Dan Fabius, VP of Clinical Informatics, Continuum Health
Here’s a quick example: Sam’s physician reports a diagnosis of diabetes, but does not report Sam’s nephropathy. The payer assigns a risk factor for diabetes. When combined with demographic data, Sam’s annual spending benchmark is $10,000. If Sam’s physician had reported both diabetes and nephropathy, the payer would have assigned a higher risk factor, and an annual spending benchmark of $18,000.
Sam’s actual cost of care for the year was $15,000. But since Sam’s physician only reported the diabetes diagnosis, Sam’s cost of care exceeded the $10,000 benchmark by $5,000. However, if both diagnoses had been reported, Sam’s cost of care would have been below the $18,000 benchmark, and his doctor would have been recognized by the payer as saving $3,000.
TOP TIP: Update diagnoses annually
Risk adjustment coding is particularly important for Medicare Advantage patients, as these plans use a detailed risk-adjustment process for each patient. In fact, every January 1, Medicare wipes the slate clean for all members: Everyone is considered completely healthy until diagnosis codes are reported.
Therefore, physicians should see their patients at least once a year (such as an annual wellness visit) and evaluate and document all conditions related to the patient’s health status annually, including chronic and status conditions (i.e., lower limb amputation). This will ensure that payer data is up-to-date and will therefore maximize the resources available to the physician and patient. If a chronic and/or status condition is not reported annually, it indicates the condition is resolved and no longer exists, leading to an inaccurate depiction of the patient’s health status and inaccurate risk scores set by the payer.
This model— known as Risk Adjustment—is the wave of the future. It’s already used by many payers, including ACA plans, Medicaid and Medicare.
Physicians who want to succeed in the brave new world of value-based healthcare must embrace these changes, as coding and documentation increasingly drive reimbursement, quality measures, and care models.
[php slug=PDF-Button]
Continuum Health can help physicians master these new requirements and guide practices through this evolving landscape. To learn more, please contact David Burke, Enterprise Sales Executive, at daburke@continuumhealth.net or (856) 701-6246.