Despite the past year of uncertainty surrounding healthcare policy, one objective has remained consistent. As payment models shift from fee-for-service to value based care, physicians are more accountable than ever for providing high quality services, while lowering the overall cost of care.
Yet today’s primary care physician (PCP) is responsible for more than the care he or she provides directly to patients under value based contracts. They are also accountable for a patient’s full continuum of care and all patient-provider encounters. Since quality and cost of care vary drastically across hospitals and providers, how can you ensure that your patients are receiving high-quality/high-value care?
Start by Analyzing Claims Data
Despite the perception that claims data has little value, nothing could be further from the truth. Claims data is the cost information for patients represented by the Centers for Medicare and Medicaid Services (CMS) or commercial payers. Claims data includes billing codes for procedures, prescriptions, hospital or specialist visits, ancillary health services, and other medical costs a patient incurs. By analyzing final payment information from various providers and sites of service, you can gain a retrospective view on a patient’s entire medical history, not just visits to your practice. It is the one single source of truth regarding healthcare utilization and costs.
Providers are not always aware of every medical encounter a patient experiences. Occasionally, patients incur high-cost emergency room visits, consult outside specialists, or visit health systems with high provider and/or facility fees. If you’re not reviewing claims data for your patient population, you may not be aware of your patients’ utilization and total cost of care.
Providers can be unknowingly penalized for high patient population costs, so analyzing claims data is crucial for identifying positive and negative trends in cost, quality, and overall healthcare utilization. To leverage these trends and develop strategies aimed at lowering cost and increasing quality, start with these three steps:
-
- Ensure proper patient attribution
Payers attribute patients to providers based on cost, geographical location, patient’s choice, and other methods. Once a population has been attributed, a provider is responsible for the plurality of care for every patient within his or her population. Unfortunately, physicians are often held responsible for patients they have never met or haven’t seen in several years, yet can still be penalized with payment adjustments.As a provider, you must review your attribution list to better understand the population’s members and gain insights into why they may have been attributed to you. Once you have this data, you can potentially dispute and correct attribution with the payer. Ultimately, you want to ensure that you’re administering quality care to the correct population and foster greater patient engagement throughout the year. - Target high-risk and rising-risk patients
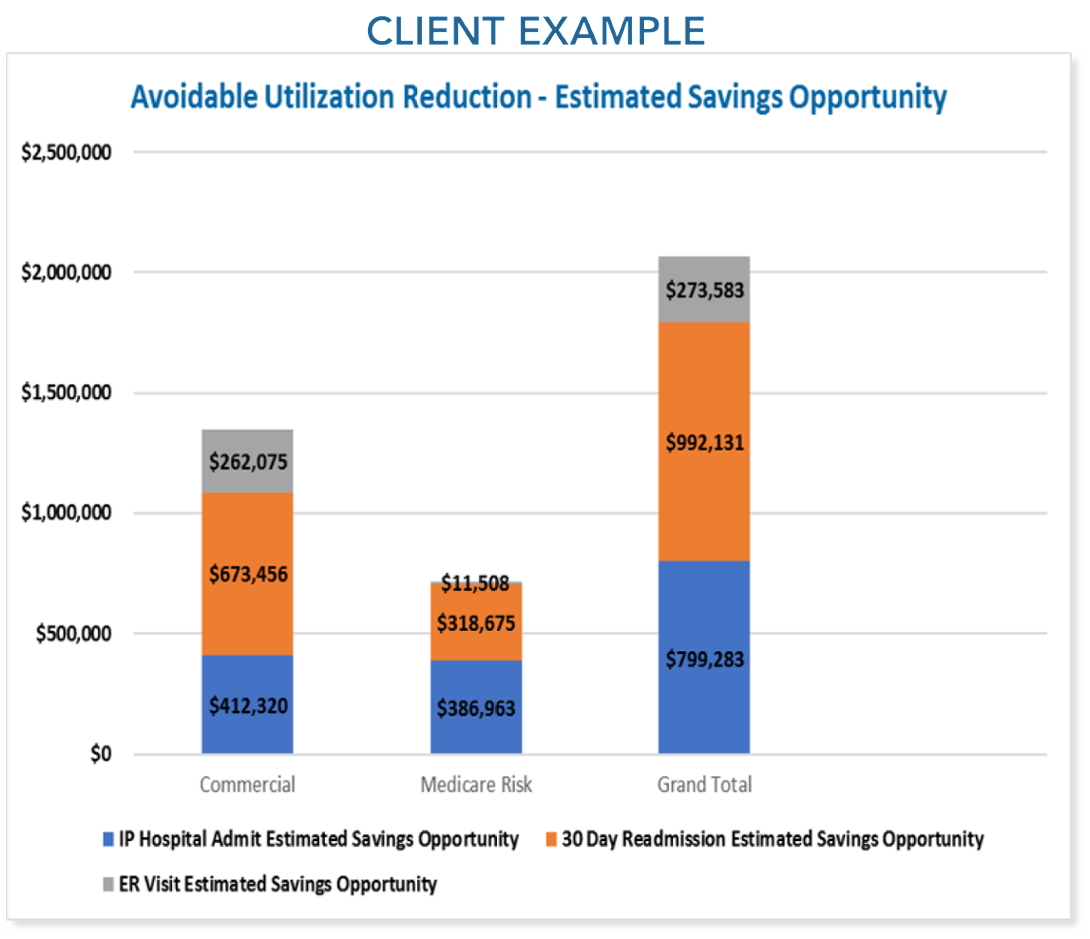
You can determine the top 3–10 percent of your high-need, high-cost patients by analyzing claims data. After identifying patients with multiple co-morbidities and high utilization, begin developing strategies for intervention and care coordination based on the medical and prescription data detailed in their claims. You can devise tactics for ensuring consistent physician visits, medication adherence, and develop methods for preventing repeat hospitalizations and avoidable ED utilization.By targeting high-risk or rising-risk patients, you can focus on improving outcomes and lowering overall healthcare costs. - Create a cost of care strategy based on empirical data
The majority of US physicians refer patients based on habitual referrals and past relationships, but only 15 percent of physicians refer based on data outcomes or quality ratings.1 Though most providers make referrals to trusted physicians and specialists, these referrals do not guarantee the highest quality care at the lowest cost.By leveraging claims data, the total cost of care for every patient in a provider’s population can be used to identify trends in cost and quality. Use claims data to determine which facilities offer the lowest costs for various medical procedures. Based on this information, aim to refer patients to quality facilities with higher value and lower the cost of care for your attributed population.
- Ensure proper patient attribution
Develop an Integrated Analytics Strategy
According to a recent Deloitte survey on effective data management, only 1 out of every 5 healthcare organizations has an integrated strategy for leveraging data analytics.2 Under the Affordable Care Act (ACA), healthcare organizations are required to report on quality, engagement, and cost. Yet even with the amount of information aggregated, organizations are not capitalizing on this data to lower cost, maximize efficiency, and coordinate care.
Providers and practices should capitalize on their existing technology and reporting systems to focus on claims data. Despite a traditional 45 to 90-day lag time between claims submission and retrospective claims data, practices can streamline the process by submitting quick, error-free claims. This increases the odds of receiving more timely claims data from the payer. By improving your claims submission process, you gain a more current picture of your patient population, while also enhancing cash flow.
Once you’ve optimized your claims process, provider groups may consider adding a data analyst to their staff or working with an outside partner to develop an integrated analytics strategy. Through this strategy, your team can focus on high quality/low cost sites of service and providers, accurate patient attribution, and coordinated care to help drive down cost.
If all this still seems challenging for your practice, consider engaging an outside partner who can help you mine claims data for value based opportunities. To learn more about Continuum Health, please call David Burke, Enterprise Sales Executive at dburke@continuumhealth.net or 856.701.6246.
1 Practicing value-based care: What do doctors need?
2 Health system analytics: The missing key to unlock value-based care